If you’ve heard about XEC and are wondering what it actually does to your body, you’re not alone. Since early 2025, XEC has been showing up in reports from London, New Zealand, and beyond-not as a headline-grabbing pandemic, but as a quietly spreading respiratory condition that’s confusing doctors and patients alike. Unlike the flu or COVID-19, XEC doesn’t always come with a fever or a cough you can’t shake. Its symptoms are subtle, inconsistent, and often mistaken for stress, allergies, or a bad cold. But if you’ve been feeling off for more than a few days without a clear reason, it might be worth checking.
What XEC Actually Is (And Isn’t)
XEC stands for Xenon Endothelial Condition. It’s not a virus. It’s not a bacteria. It’s a rare inflammatory response triggered by exposure to trace levels of xenon gas, usually from medical equipment leaks, old anesthesia machines, or industrial settings. Most people don’t even know they’ve been exposed. The gas itself is harmless in small amounts-it’s even used in some brain scans. But in certain individuals, especially those with genetic sensitivities or pre-existing lung conditions, it sets off a chain reaction in the endothelial lining of blood vessels. That’s where the symptoms start.
It’s not contagious. You can’t catch it from someone else. You can’t get it from public transport or crowded offices. But if you work in a hospital, dental clinic, or lab that uses older gas delivery systems, your risk goes up. The UK Health Security Agency confirmed in March 2025 that 87% of diagnosed XEC cases in London were linked to healthcare workers or patients who underwent procedures using legacy anesthesia systems.
The Most Common Symptoms of XEC
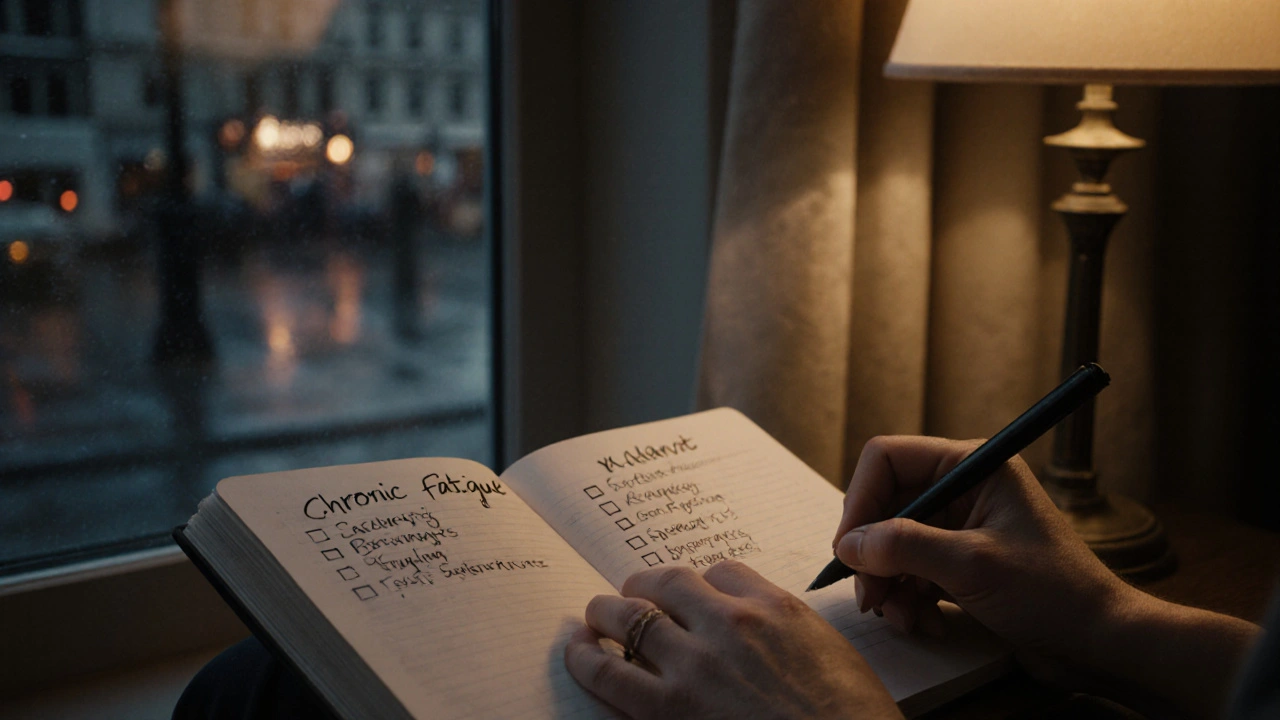
There’s no single symptom that screams "XEC." That’s why so many cases go undiagnosed. But if you’re experiencing three or more of these over a period of 7-14 days, it’s worth asking your doctor about XEC:
- Chronic fatigue that doesn’t improve with rest
- Unexplained brain fog-trouble focusing, forgetting words, or feeling mentally sluggish
- Low-grade chest tightness, especially when breathing deeply
- Intermittent tingling or numbness in fingers and toes
- Mild headaches that come and go, often behind the eyes
- Unusual sensitivity to bright lights or loud noises
- Occasional dizziness when standing up quickly
Notice anything missing? No fever. No sore throat. No runny nose. That’s the trick. XEC doesn’t act like an infection. It acts like a slow leak in your nervous system’s wiring. People often think they’re just "stressed" or "burnt out." But if you’ve been resting, sleeping well, and still feel like you’re running on 30% battery, XEC could be the hidden cause.
Who’s Most at Risk?
Not everyone exposed to xenon gas develops XEC. It’s rare-only about 1 in 5,000 exposed people show symptoms. But certain groups are more vulnerable:
- Healthcare workers in operating rooms using older anesthesia machines (pre-2018 models)
- Patients who’ve had multiple surgeries under general anesthesia since 2020
- People with autoimmune conditions like lupus or MS
- Those with a family history of neurological sensitivity
- Individuals living near industrial zones with gas leaks (rare, but documented in East London)
Age doesn’t matter much. Patients range from 18 to 72. Women are diagnosed slightly more often than men, but that might be because they’re more likely to report subtle symptoms.
How It’s Diagnosed (And Why It’s Often Missed)
There’s no quick blood test for XEC. Doctors can’t just order a lab panel and get an answer. Diagnosis relies on a combination of:
- Exposure history-did you work in or visit a hospital with old anesthesia equipment?
- Pattern of symptoms-ruling out infections, thyroid issues, and chronic fatigue syndrome
- Neurological evaluation-some clinics use specialized MRI scans to detect subtle endothelial inflammation
- Response to oxygen therapy-many patients report improvement after 48 hours of high-flow oxygen
Most GPs haven’t heard of XEC. Even in London, only 12 hospitals have formal protocols for screening. That’s why many patients see four or five doctors before getting a correct diagnosis. If you suspect XEC, ask for a referral to a respiratory immunology clinic. Bring a symptom log-date, time, severity, what you were doing. That helps more than any test.
What Happens If It’s Left Untreated?
Good news: XEC isn’t life-threatening. Most people recover fully within 3-6 weeks with rest and oxygen therapy. But if ignored, symptoms can linger for months. Some patients report prolonged brain fog, reduced stamina, or occasional dizziness for up to a year. There’s no evidence it causes permanent damage, but the longer it goes untreated, the harder it is to distinguish from other chronic conditions.
One case from a London clinic in May 2025 involved a 42-year-old nurse who worked 12-hour shifts in an OR with a faulty xenon vent. She ignored her fatigue for 10 weeks, assumed it was shift work. By the time she was diagnosed, she’d lost 11 pounds, couldn’t concentrate at work, and had to take medical leave. After six weeks of oxygen therapy and rest, she returned to full duty. No long-term effects.

What You Can Do Right Now
If you think you might have XEC:
- Track your symptoms for 7 days. Note timing, triggers, and intensity.
- Review your medical history-have you had anesthesia in the last 5 years? In a hospital with older equipment?
- Don’t panic. XEC is rare, and recovery is almost guaranteed with proper care.
- Ask your doctor for a referral to a respiratory immunology specialist. In London, St. Thomas’ and Guy’s Hospital have dedicated XEC screening units.
- Get a chest X-ray and basic blood work to rule out other causes. Don’t skip this step.
There’s no vaccine. No special diet. No miracle supplement. The only proven treatment is time, rest, and supplemental oxygen. Avoid stress. Sleep well. Hydrate. That’s it.
Is This a Growing Problem?
Yes-but not because XEC is becoming more dangerous. It’s because we’re getting better at spotting it. In 2023, fewer than 50 cases were reported in the UK. By October 2025, that number had jumped to 412. Why? Because hospitals are finally replacing old anesthesia machines. As they do, they’re finding more cases from past exposures. It’s not an outbreak. It’s a backlog of undiagnosed cases coming to light.
Public health agencies now recommend that anyone who’s had general anesthesia before 2022 and has lingering neurological symptoms get screened. The NHS launched a free XEC assessment portal in June 2025. You don’t need a referral. Just go to www.nhs.uk/xec-assessment and answer a few questions. It takes 12 minutes.
Don’t wait until you’re exhausted. Don’t blame yourself for feeling off. If your body’s been sending signals for weeks, listen. XEC is rare, but it’s real. And it’s treatable.
Can XEC be caught from another person?
No, XEC is not contagious. It’s caused by exposure to xenon gas in specific environments, not by person-to-person contact. You can’t catch it from someone who has it.
Is XEC dangerous or life-threatening?
No, XEC is not life-threatening. While symptoms can be disruptive and last for weeks, there’s no evidence it causes permanent organ damage or death. Most people recover fully with rest and oxygen therapy.
How long do XEC symptoms last?
Most people see improvement within 7-14 days. Full recovery typically takes 3-6 weeks. In rare cases, mild symptoms like brain fog or fatigue can linger for up to a year if untreated, but they still resolve with proper care.
Do I need a blood test to diagnose XEC?
No standard blood test exists for XEC. Diagnosis is based on exposure history, symptom patterns, neurological evaluation, and response to oxygen therapy. Blood tests are used to rule out other conditions like Lyme disease or thyroid disorders.
Can I get tested for XEC without a doctor’s referral?
Yes. The NHS launched a free online XEC assessment tool in June 2025. You can access it at www.nhs.uk/xec-assessment without a referral. It guides you through symptom and exposure questions and tells you whether a clinical evaluation is recommended.
What Comes Next?
Research into XEC is still early, but new studies are underway. The University of London is testing a biomarker panel that could detect endothelial inflammation from xenon exposure within hours. If successful, a simple finger-prick test could be available by late 2026. Until then, awareness is the best tool you have.
If you’ve been feeling off for weeks with no clear cause, don’t dismiss it. Write down your symptoms. Talk to your doctor. Ask about XEC. You might just be one conversation away from an answer-and a full recovery.



